Data Management for Health Parity
Data Management for Health Parity
The State of Colorado continuously seeks innovative approaches to accurately identify members between our programs and to better understand and support interventions to address health disparities. In support of the Colorado Health IT Roadmaps, led by OeHI and steered by the eHealth Commission, the state established a statewide initiative to improve this process and enhance technology where appropriate. These improvements will result in better access to care, lower cost of care, and improved quality of care for all Coloradans.
Identity Cross Reference Service (IDXR)
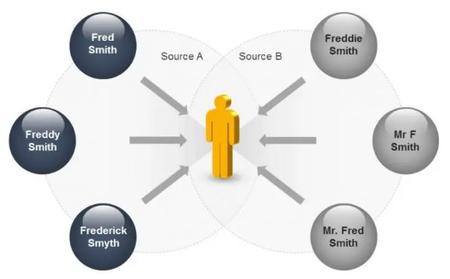
As health and human service providers have become more interconnected, so too have the IT systems that support those providers. Many of these systems were initially designed to address specific problems and were not intended to interoperate with one another. This resulted in patients/clients having individual profiles in each system without a means to connect those profiles between the systems. Identity resolution is the process of using information provided by an individual to identify them uniquely and accurately across multiple systems.
IDXR supports the:
- Interoperability and scalability between systems
- Identification of data quality issues
- Creation of a Master Data Management (MDM) solution
Data Management for Health Parity Projects at OeHI
Cross Reference Lookup
The process of cross-reference look up establishes a unique digital identity of individual members across State healthcare systems and Colorado’s health information exchange (HIE). Colorado’s HIE supplies new patient demographic data as part of the identity resolution process, offering the ability for care coordinators and primary care medical providers to develop personalized care plans.
Standardized data collection with safeguards for privacy and confidentiality is critically important in the effort to understand and eliminate racial and ethnic disparities in health care.
Demographic Enrichment
Enhancing a patient’s base identity with demographic data enhances the capacity of the Colorado health programs to bring together multiple data sources at the point of care to illuminate health disparities.
Having data on member race and ethnicity will allow health professionals to better disentangle factors that are associated with health care disparities. Further, collecting and analyzing patterns of health care by member race, ethnicity, and other demographic data can help the Department to monitor the quality of care provided by its provider networks. Such monitoring can help to ensure accountability to enrolled members, improve member choice, and allow for evaluation of intervention programs, all with the ultimate goal of improving health parity.
Vaccinations and COVID
The Colorado Department of Health Care Policy and Financing(HCPF) regularly requests Immunization records from the Colorado Department of Public Health and Environment(CDPHE). CDPHE stores immunization data that has been reported in the Colorado Immunization Information System(CIIS) production system. The Colorado Electronic Disease Reporting System(CEDRS) contains data pertaining to diseases reported, diagnosis made and course of action for treating the disease. Enrichment of data elements in CDPHE CIIS patient records improve the accuracy of Health Equity for Vaccine status reporting and enabling coordinated outreach to their unvaccinated population to encourage them to become vaccinated.
Recommendations to Support the Data Landscape of Colorado's Local Public Health Agencies (LPHAs)-This resource, provided by the Colorado Office of eHealth Innovation, recommends action steps, backed by state-wide stakeholder interviews, that the State of Colorado can pursue to improve the data sharing landscape for LPHA's in Colorado.